Exploring OCD vs OCPD and Distinguishing Features
Exploring OCD vs OCPD
Obsessive-compulsive personality disorder (OCPD) is often misunderstood and misdiagnosed. Yet, it is one of the most common personality disorders (Rizvi, 2023). One of the conditions OCPD is often confused with is obsessive compulsive disorder (OCD), a more commonly understood — but also undertreated condition (Senter, 2021). And, to add another layer of complexity to this overshadowed condition, even though OCPD and autism have distinctly separate diagnostic criteria, they too share overlapping traits (Gadelkarim, 2020) presenting some real challenges for clinicians supporting neurodivergent folks!
As an Autistic psychologist with OCD I’m invested in exploring the intricacies of complex conditions, neurodivergence, and their misdiagnosis, this article aims to take a deeper dive into OCPD vs OCD, how the conditions vary and their distinguishing features, and provides answers to some commonly asked questions about OCD and OCPD.
Contents:
What is OCD?
Obsessive compulsive disorder (commonly known as OCD), is characterized by a cycle of obsessions and compulsions that persist despite being disproportiate, or unhelpful, to the situation. Obsessions and compulsions live in cyclical relationship to one another. More specifically:
Obsessions: Recurrent and persistent thoughts, urges, or images, and compulsions that are intrusive or unwanted and cause anxiety or distress
Compulsions: Repetitive behaviors or mental acts — e.g. hand washing, or checking — in response to the obsession, in an attempt to ignore or suppress these thoughts, urges, or images and alleviate the anxiety related to these obsessions
In a real-life context, this might look like: experiencing beleaguering thoughts — such as a persistent and intense fear of contamination in public places – and responding with a compulsion in your attempt to rid yourself of the anxiety. For example, as a child, when I experienced an OCD intrusive thought, or thought I did something wrong, I would immediately say the salvation prayer “Jesus, come into my heart and save me,” this would rid me of the sense of badness until another bad thought came. The Jesus prayer (compulsion) functioned to neutralize (reduce) the feeling of badness (obsession).
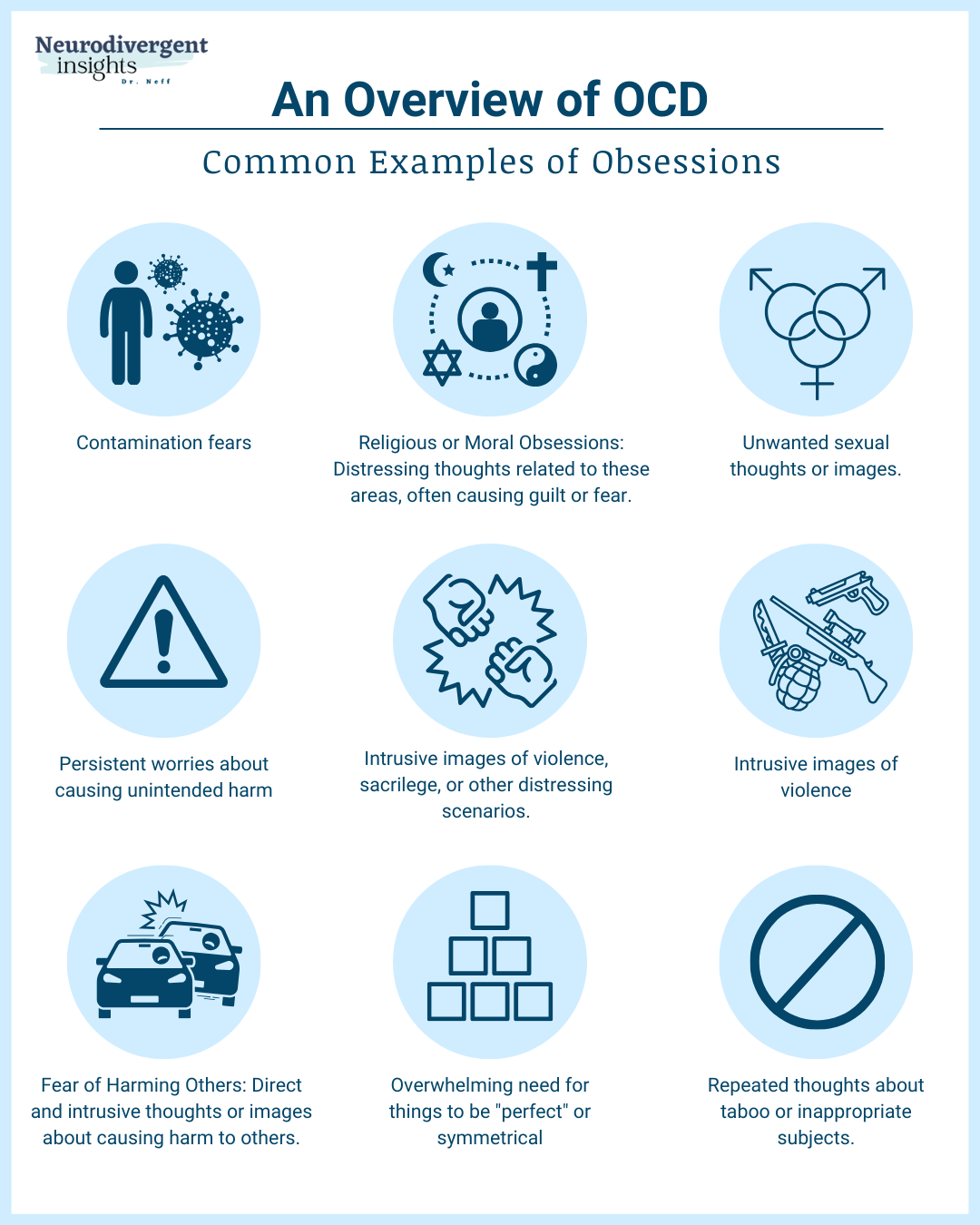
I’ve listed some common obsessions and compulsions below, and you can read more detailed information in my blog What is Obsessive Compulsive Disorder?
Examples of Common Obsessions
Fear of contamination
Persistent worries about safety
Fear or sickness
Hoarding
Fear or losing control
Symmetry and order
Sexual obsessions
Superstition
Religious or moral obsessions
Unwanted and intrusive sexual imagery
Unwanted and intrusive images of violence
Persistent worries of causing harm to others
Repeated thoughts about taboo or inappropriate subjects
Excessive rumination on existential themes, such as the meaning of life, death, or the nature of reality
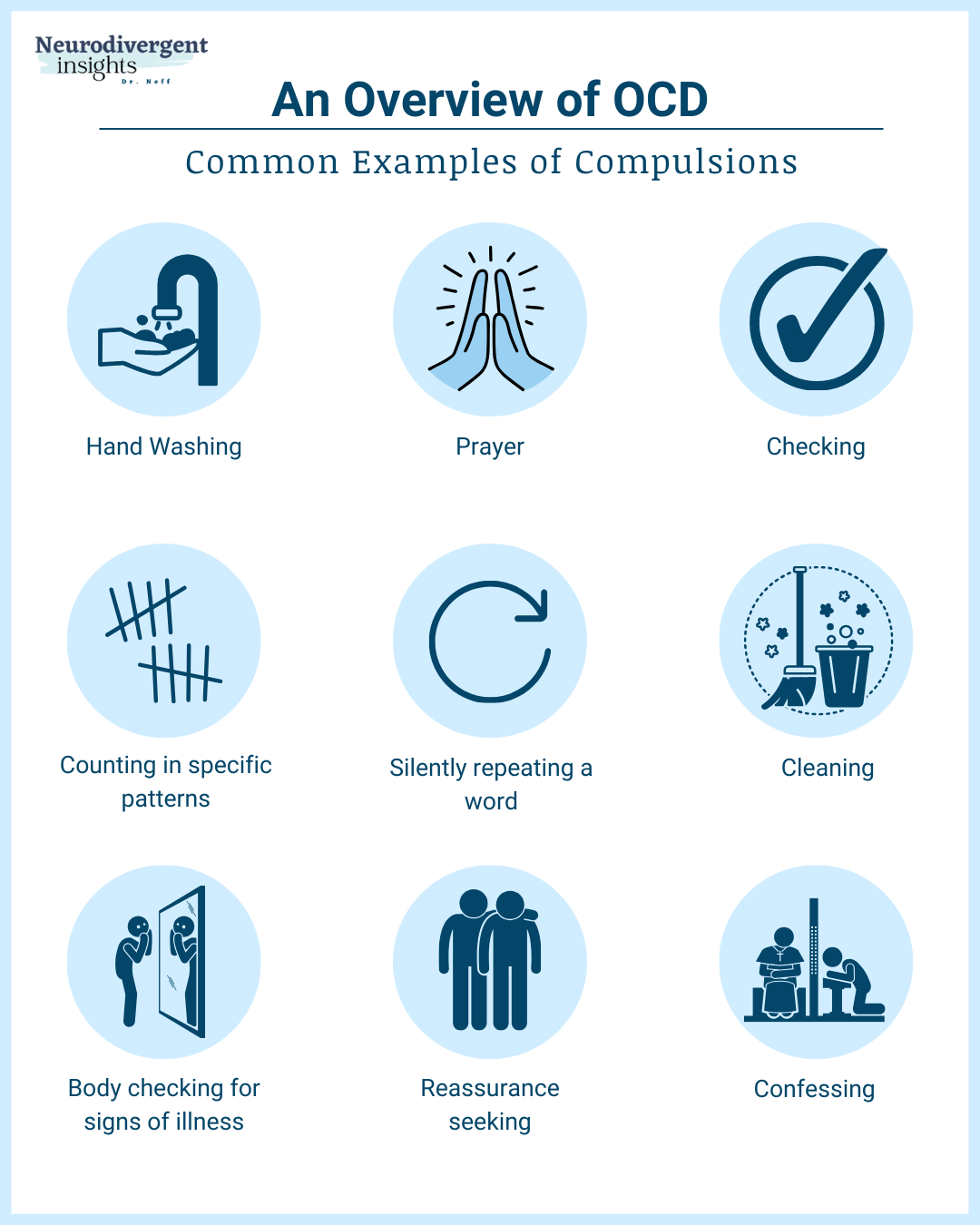
Examples of Common Compulsions
Checking and re-checking
Counting
Handwashing
Repeating words or phrases
Arranging and ordering
Repeated mental rituals
Repetitive thoughts to counteract the obsessive thoughts
Repetitive prayer
Cleaning
Confessing
Reassurance seeking
Body checks for signs of illness
OCD Co-occurrence and Prevalence
OCD impacts 2 to 3 percent of Americans (American Psychiatric Association, 2022) with studies demonstrating that OCD is familial, partially due to genetic factors (Pauls, 2022). For folks with neurodivergence, particularly ADHD and autism, rates of OCD is much more common and it can be more tricky to tease them apart, which you can read more about here. OCD is also more common among people with OCPD. The range of prevalence have found a co-occurrence of between 23-32% (Lochner et al., 2011).
Distinguishing Features of OCD
Given OCD co-occurs so often with autism, ADHD and OCPD it can be difficult to tease it a part. To distinguish OCD from these other conditions, there are two distinguishing features that can be helpful:
1) The Relationship between obsessions and compulsions
2) The Ego-dystonic nature of OCD
The Obsession-Compulsion Loop
First, obsessions and compulsions within OCD form a tight loop. This is part of what makes OCD a sneaky trap to walk out of. Compulsions can look a lot like an OCPD need for control, it can also look a lot like Autistic rituals. However, when it’s an OCD compulsion it will be tightly connected to an obsession. For example:
A contamination obsession leads to compulsive hand washing to reduce the contamination obsession.
The obsession with the possibility of causing accidental harm may lead to compulsively checking appliances or locks multiple times to ensure safety.
An obsession with objects being perfectly aligned and symmetrical can result in the compulsion to arrange and rearrange items until they feel “just right.”
The obsessive fear of being immoral or sinful may compel a person to seek frequent confession or reassurance, even for thoughts or actions that are universally considered trivial.
An obsession with having a serious illness might lead to compulsive behaviors such as repeatedly researching medical information online or seeking numerous medical opinions.
An obsession with losing items that might be needed in the future can drive the compulsion to hoard items, often leading to an excessive accumulation of possessions.
Obsessive unwanted intrusive thoughts may lead to mental compulsions, such as repeating certain words or phrases to neutralize or counteract the anxiety-inducing thought.
An obsession with making social mistakes or being judged negatively can lead to compulsively seeking reassurance from others about one's social interactions.
OCD is Ego-Dystonic
One of OCD’s core distinguishing feature is that it is ego-dystonic. Ego-dystonic refers to the way in which the disorder’s symptoms—obsessive thoughts and compulsive actions—are in conflict with the person’s self-perception and values. This means that people with OCD typically recognize that their obsessions and compulsions are irrational and not aligned with their true beliefs and desires. They are aware that their repetitive thoughts and behaviors do not make logical sense, yet they feel compelled to perform them. It is this internal conflict, this mismatch between their intrusive thoughts or ritualistic behaviors and their own sense of what is rational, that leads to significant anxiety and emotional distress (Vaghi, 2019).
Here is an example from my personal life. Each Saturday I send a newsletter to about 25,000 readers, which triggers an irrational yet compelling fear: what if I've attached an inappropriate image or document by mistake? I then get sucked into a loop of checking of the URL links multiple times. Despite knowing I own no such images, this fear illustrates the ego-dystonic nature of my OCD—my actions feel disconnected from my core self. Despite my rational understanding, I'm caught in a loop of checking the email and its links multiple times. This compulsive behavior, knowing it's illogical yet feeling unable to resist, is both unhelpful (maladaptive) and distressing. It highlights how OCD compulsions clash with logic, consuming time and energy without reason, and amplifying anxiety despite understanding their irrationality. This captures the essence of OCD's disruptive impact.
Conversely, (OCPD) is ego-syntonic, meaning people with OCPD generally perceive their actions as rational and justified. Unlike my clear awareness of the irrationality in checking email links five times due to OCD, people with OCPD believe their meticulous methods or strict routines are logical and often necessary. This perspective is typical of personality disorders, where the pervasive nature of these conditions integrates into one's identity, making the behaviors, thoughts, or experiences feel natural and justified. Consequently, it can be challenging for those with OCPD to see how their actions might be excessive or how they could negatively affect themselves or others. This intrinsic alignment with one's self-image contributes to a lack of insight into the impact OCPD is having on the person. But, I’ll explain more about that lack of awareness, but first I’ll explore OCPD and how it presents.
What is OCPD?
When I think about OCPD, I picture a misunderstood distant cousin in a family tree: someone vaguely identifiable, but not really known. OCPD is poorly understood within the world at large. Even though it is poorly understood and under researched, OCPD is clinically significant as one of the most common personality disorders (Rizvi, 2023).
OCPD can be perceived as a sophisticated defense structure within the personality, one that develops over time to safeguard against feelings of vulnerability. The pursuit of perfection and the need to maintain control are behaviors employed to protect oneself from shame and the anxiety of potential chaos. Living with OCPD often feels like being overshadowed by an impending sense of doom and a persistent state of doubt, even while maintaining an outward appearance of efficiency and success. For a more comprehensive exploration of these characteristics and how they compare to autism, you can find an in-depth discussion in my detailed analysis here.
In terms of key diagnostic criteria, OCPD is marked by these characteristics (OCD International, 2010):
Unwillingness to delegate responsibilities to others
An overwhelming need for order
Rigid adherence to rules and regulations
A strong sense of control, or righteousness, about the way things “should be done”
OCPD Symptoms Include:
To qualify for an OCPD diagnosis, individuals must display at least four of the following traits, typically emerging in late adolescence or early adulthood, that persist across different environments and cause substantial distress:
Focused on Details, Order, and Rules: An intense focus on minor details, strict rule observance, and an overarching need for order, even if it means losing sight of the overall purpose.
Perfectionism that Impedes Task Fulfillment: An obsession with flawlessness that obstructs the completion of tasks, often leading to delays, unmet deadlines, or shying away from projects for fear of imperfection.
Overcommitment to Work, Overlooking Recreation and Relationships: A persistent fixation on work to the extent of forgoing downtime and neglecting personal connections.
Rigid Views on Morality and Principles: A strict commitment to personal codes of morality and principles, which can lead to judgmental perspectives and discord.
Challenges with Disposing of Nonessential or Old Items: A hard time discarding items that no longer serve a practical purpose, frequently out of a sense of duty or a concern for waste.
Hesitance to Share Tasks: Due to perfectionistic tendencies and concern over the accuracy of others' work, there is a preference for taking on excessive responsibilities with the belief that tasks are best done personally.
Thrifty Spending Approaches: An extreme hesitation to spend, to the point of self-denial, often motivated by fears of financial uncertainty.
Stiffness and Intractability: A strict commitment to one's own routines, an aversion to changes, and challenges in accommodating new environments or differing opinions.
A diagnosis of OCPD is made when these behaviors significantly impact social, familial, or occupational functioning. It's important to note that these symptoms represent a range within OCPD, and not all individuals will exhibit every trait. The diversity in symptom and the many ways it can manifest is one of the reasons this condition is poorly understood.
It’s also worth noting that these criteria are often narrow and poorly capture the OCPD experience. OCPD can have different subtypes, and this strict adherence to control and perfectionism may show up in one domain in a person’s life but not others (for example in work or in relationships). You can read more depth over-view of the OCPD subtypes over here.
Co-occurrence and Prevalence Rates
OCPD has an estimated lifetime prevalence rate between 3 and 8 percent among the general population and higher rates found in clinical settings: 8.7 percent in outpatient environments and 23.3 percent reported in inpatient settings (Rizvi, 2023). OCPD International (2010) estimates that to be 1 in 10 Americans and it is diagnosed in twice as many men as women.
OCPD Co-occurrence
OCPD is more prevalent among neurodivergent people, those with OCD, and some other conditions that share similar traits. Specifically:
OCPD and autism: OCPDs overlapping traits with autism include a preference for routine, difficulties adapting to change, and a focus on details. One study reported 54 percent of adults with OCPD also met criteria for autism (Gadelkarim, 2019)
OCD and OCPD: Other research suggests that OCPD occurs in people with OCD about 15 percent to 28 percent of the time (Thamby, 2019)
OCPD and anorexia: evidence suggests a relationship between OCPD and anorexia nervosa and binge eating disorder, particularly in areas of excessive exercise, perfectionism, and rigidity (Starcevic, 2014; Young, 2013)
OCPD, OCD, and ADHD: symptoms of COPD were associated with higher levels impulsivity in ADHD and OCD in internet use (Chamberlain, 2017)
OCPD, depressive disorder, and suicidal ideation: while there are some studies showing a co-occurrence between OCPD and depression, data was inconsistent. However, OCPD was linked to depressive disorder and increased rates of current lifetime suicidal ideation and suicide attempts (Starcevic, 2014).
You can read more about the overlapping symptoms and distinguishing features of OCPD vs autism in my article, here.
Can You Have OCD and OCPD?
Even though OCD and OCPD are different conditions, they do share some characteristics. Early studies hint that both might be connected to how serotonin, a chemical in our brain, works in specific areas like the prefrontal cortex and amygdala. These brain regions play a big role in how we make decisions, form habits, and control our emotions (Rizvi, 2023).
It is possible to have OCPD and OCD. Research suggests that 15 to 28 percent of individuals with OCD also have OCPD (Thamby, 2019). Both conditions are easily confused for one another because they share similarities in obsessive traits and a desire for control. However, individuals with OCD are compelled by a need to silence their obsessions and reduce their anxiety. In contrast, those with OCPD are often driven by an underlying need to protect themselves from the shame of flaws or imperfections. I’ll explore these key differences next.
What is the Difference Between OCD and OCPD?
The key differences between OCD and OCPD include:
Individuals with OCPD are often not aware they have a personality disorder — there thoughts, attitudes, and behaviors are consistent with their self-image or perceived as rational, helpful, or desirable (this is also referred to as ego-syntonic). Whereas OCD is ego-dystonic, meaning the person is aware about their obsessions and compulsions and they are experienced as inconsistent with their self-perception / core self.
Due to ego-syntonic nature of OCPD, a person with OCPD may be more likely to act on impulses, and/or cause harm to themselves or others
People with OCD actively try to control, or neutralize their obsessions, whereas people with OCPD are motivated by protecting against perceived faults or flaws.
OCD is less prevalent than OCPD, affecting 2 to 3 percent of the population, whereas OCPD impacts around 3-8 percent of the general population (American Psychiatric Association, 2022; Rizvi, 2023)
OCPD is characterized by a focus on work or control and OCD may be more focused on rituals and repetitive compulsions.
OCD follows a distinct obsessive-compulsive loop that can be difficult to break.
OCPD is a personality disorder, meaning that a defense structure has formed around the personality. And this case for the protection against perceived flaws and vulnerabilities.
Treatment Differences Between OCD and OCPD
There are treatment similarities and differences between OCD and OCPD.
Interventions for OCPD and OCD:
Psychotherapy to break cycles of obsessive behavior
Medication (selective serotonin reuptake inhibitors (SSRIs) to alleviate anxiety and intrusive thoughts, enabling the person to engage in therapy. However, there is less research about the use of SSRIs as a treatment option for people with OCPD, but some research shows they have been supportive (Thamby, 2019)
OCD treatments:
Inference-based Cognitive-Behavior Therapy (I-CBT)
Exposure and response prevention (ERP)
Eye movement desensitization and reprocessing (EMDR) has shown potential in addressing memories associated with OCD
OCPD interventions:
Relaxation techniques have been used for OCPD, to reduce a sense of urgency and stress
Schema therapy
OCD and OCPD Resources
If you want to delve further into OCD and OCPD, I've listed some resources below that you might find helpful, including several recently published books and fact sheets.
Obsessive Compulsive Personality Disorder vs autism: one of my recent articles exploring neurodivergence and OCPD
Exploring the Overlap: OCD and the Neurodivergent Mind: in this article I provide more detailed information about the intersection between OCD and ADHD and/or autism
What is Obsessive Compulsive Disorder: I’ve explored OCD in greater detail in this article
Misdiagnosis Monday: an exploration of commonly misunderstood and misdiagnosed conditions. You’ll also find two books I’ve written on ADHD and OCD and autism and OCD
OCPD Fact Sheet: detailed information from the CDC about OCPD
Obsessive-Compulsive Personality Test: a helpful screening tool for OCPD (but not a substitute for professional diagnosis)
The OCPD Foundation: a supportive community with resources for individuals with OCPD
OCPD Deep Dive by Dr. Honda: a podcast offering in-depth conversations about personality disorders
The Self-Compassion Workbook for OCD: recommended among clinicians for being neurodivergent affirming
OCD Daniel: a book for teens and children that normalizes OCD
What to Do When Your Brain Gets Stuck: A Kid’s Guide to Overcoming OCD: I found this book the most helpful when one of my children was struggling with OCD
Summary and Conclusion
Through exploring the intricate world of OCD and OCPD, it's clear these conditions share intersecting traits, with a desire for routine, ritual, focus, and difficulty with change. However, the underlying motivations and experiences are distinctly different. OCD is an anxiety disorder, motivated by a desire to neutralize obsessive and intrusive thoughts; OCPD is a personality disorder driven by a strong desire for control, perfectionism and protection against flaw shame.
What complicates diagnosis and treatment isn’t just the overlapping traits, it’s their co-occurrence, lack of accurate (and often late diagnosis) and understanding of these conditions collectively. This highlights the need for clinicians to better understand the nuance, motivation, and complexity of these interwoven disorders to provide effective, empathetic, and tailored solutions to meet the needs of clients.
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Publishing.
What is obsessive-compulsive disorder?. Psychiatry.org - What Is Obsessive-Compulsive Disorder? (2022, October). https://www.psychiatry.org/patients-families/obsessive-compulsive-disorder/what-is-obsessive-compulsive-disorder
Brem, S., Grünblatt, E., Drechsler, R., Riederer, P., & Walitza, S. (2014). The neurobiological link between OCD and ADHD. Attention deficit and hyperactivity disorders, 6(3), 175–202. https://doi.org/10.1007/s12402-014-0146-x
Chamberlain, S. R., Redden, S. A., Stein, D. J., Lochner, C., & Grant, J. E. (2017). Impact of obsessive-compulsive personality disorder symptoms in Internet users. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists, 29(3), 173–181.
Gadelkarim, W., Shahper, S., Reid, J., Wikramanayake, M., Kaur, S., Kolli, S., ... & Osman, S. (2017). Obsessive compulsive personality disorder and autism spectrum disorder traits in the obsessive-compulsive disorder clinic. European Psychiatry, 41(S1), S135-S136.
Masi, G., Millepiedi, S., Perugi, G., Pfanner, C., Berloffa, S., Pari, C., Mucci, M., & Akiskal, H. S. (2010). A naturalistic exploratory study of the impact of demographic, phenotypic and comorbid features in pediatric obsessive-compulsive disorder. Psychopathology, 43(2), 69–78. https://doi.org/10.1159/000274175
Meier, S. M., Petersen, L., Schendel, D. E., Mattheisen, M., Mortensen, P. B., & Mors, O. (2015). Obsessive-Compulsive Disorder and autism Spectrum Disorders: Longitudinal and Offspring Risk. PloS one, 10(11), e0141703. https://doi.org/10.1371/journal.pone.0141703
Pauls, D., L. (2010) The genetics of obsessive-compulsive disorder: A review. Dialogues in Clinical Neuroscience, 12:2, 149-163. DOI: 10.31887/DCNS.2010.12.2/dpauls
Rizvi A, Torrico TJ. Obsessive-Compulsive Personality Disorder. [Updated 2023 Oct 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK597372/
Senter, M. S., Search for more papers by this author, Patel, S. R., Dixon, L. B., Myers, R. W., Simpson, H. B., New York State Psychiatric Institute and Department of Psychiatry, Send correspondence to Dr. Patel ([email protected])., AM, R., Al., E., AC, K., SM, M., NA, F., LM, K., EB, F., HB, S., SG, F., G, G.-S., E, H., … I, N. (2021, May 7). Defining and addressing gaps in care for obsessive-compulsive disorder in the United States. Psychiatric Services. https://ps.psychiatryonline.org/doi/10.1176/appi.ps.202000296
Starcevic V, Brakoulias V. (2014). New diagnostic perspectives on obsessive-compulsive personality disorder and its links with other conditions. Curr Opin Psychiatry, 27(1): 62-7. DOI: 10.1097/YCO.0000000000000030.